6 ways to improve mental health access: What really works?

You see these gaps every day. Clients struggle with cost, long wait times, and finding care that fits their needs. As a therapist, you’re on the front lines of a mental health system that often fails the people it’s meant to serve.
We asked more than 1,300 therapists how they would solve access and equity in mental healthcare for our Future of Therapy report. The solutions ranged from big policy changes to specific community programs. 30% recommend insurance reform or universal coverage, 20% would make care more affordable, 11% would integrate mental health care into schools and communities, 3% would create big policies or system reforms, 2% would improve telehealth and tech access, and 1% would improve cultural and language access.
But how realistic are these solutions? What stands in the way, and where have they worked? Here’s a clear look at each, highlighting what’s possible and what needs hard work.
1. Insurance reform and universal coverage
30% of the therapists we surveyed believe that improving insurance systems and expanding coverage are critical steps towards addressing mental health care access challenges.
Universal coverage, which ensures that everyone has access to healthcare regardless of employment, income, or pre-existing conditions, is a foundational concept. Countries like England and New Zealand integrate both mental and physical health care under national systems, funding outpatient visits, medications, and community-based supports. However, these systems, even when operational, face issues like long wait times, insufficient workforce capacity, and persisting equity gaps.
Expanding insurance coverage, such as Medicaid under the Affordable Care Act (ACA), has demonstrated some success in increasing outpatient care access. Evidence shows that white and Hispanic adults saw improved utilization, but Black adults remained disproportionately underserved, highlighting deeper structural barriers.
Mental health parity laws, designed to ensure equal coverage for mental and physical health services, have also struggled due to poor enforcement. Patients often face out-of-network denials or higher costs for therapy compared to physical health care, which underscores the limits of parity laws when oversight is weak.
Achieving universal coverage in the U.S. poses significant logistical and political challenges. A single-payer system or full-scale universal coverage would require decades of effort, steady funding, and bipartisan support.
True universal coverage, like a single-payer system, faces major political hurdles in the U.S. Even in countries that have it, like the UK or New Zealand, the system took decades to build and hinges on strong political support, steady funding, and a workforce willing to meet increased demand. However, smaller, more targeted steps, like enforcing parity laws, improving insurer accountability, and expanding Medicaid, are achievable. Aggressively enforcing existing parity laws and pushing states to reject health plans with “ghost networks” (lists of providers who aren’t actually available) can make a real difference. For you, this means supporting advocacy groups that hold insurers accountable. While these incremental efforts show promise, they rely on strong oversight and funding to address systemic inequities such as structural racism and workforce shortages.
Despite these hurdles, universal coverage and reforming insurance practices can reduce financial barriers, increase access to services, and promote early intervention, delivering long-term cost savings and improved health outcomes. However, to achieve equity, such reforms must be paired with substantial investments in mental health infrastructure, anti-racism initiatives, and community-centered approaches to ensure inclusive and effective care for all populations.
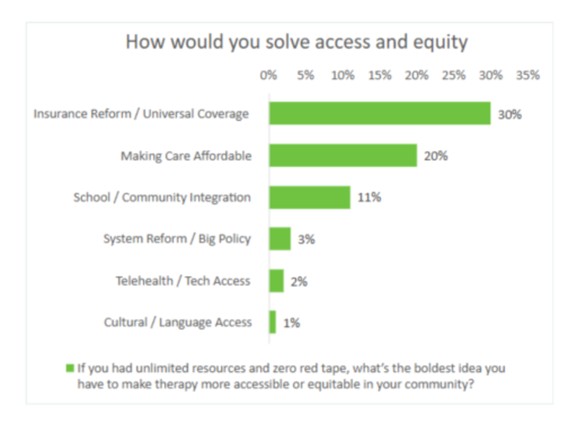
2. Making care more affordable
Reducing the direct cost of mental health care remains a critical step in improving access to treatment. High out-of-pocket expenses, such as copays, deductibles, and out-of-network fees, are some of the most significant barriers that deter individuals from seeking care or continuing treatment. Therapists have long recognized this issue, with 20% of those surveyed in the Future of Therapy report identifying affordability as a top priority for reform. Evidence consistently shows that when care is affordable, clients are more likely to attend sessions consistently, adhere to treatment plans, and achieve better outcomes.
However, lowering costs for clients brings its own challenges. For instance, reduced out-of-pocket expenses often correlate with lower reimbursement rates for therapists, making it financially unsustainable for many to accept insurance. This cycle discourages therapists from joining networks, contributes to workforce shortages, and strains existing providers. Additionally, without adequate therapists available within insurance networks, even affordable care becomes inaccessible to many.
Addressing these challenges involves striking a balance. Raising reimbursement rates for mental health services to align with those for physical health can incentivize providers to join networks while ensuring clients benefit from affordable care. States like Oregon and Massachusetts are exploring policies such as minimum fee schedules for behavioral health services, demonstrating how systemic changes can simultaneously support therapists and clients. A similar approach was observed in Virginia, where increased Medicaid reimbursement rates led to greater access to treatment for opioid use disorders and a reduction in emergency visits, proving the tangible benefits of such reforms.
While affordability can significantly increase access to mental health care, the effort must be paired with systemic investments to expand the workforce, enforce equitable pay, and support provider sustainability. Only by creating a comprehensive and balanced framework can we ensure that affordable mental health care reaches all those in need.
3. Integrating care into schools and communities
About 11% of therapists surveyed for the Future of Therapy report suggested delivering care directly to schools and local communities. This strategy reduces stigma, removes barriers like transportation, and makes mental health services easier to access. Evidence for this model is clear: school and community-based programs have shown significant success globally and in the US, especially for young people and high-risk groups.
Providing mental health support in schools is one of the most equitable ways to reach children and adolescents. School-based health services ensure the majority of students, especially those from low-income families, can access help without needing to travel or overcome logistical hurdles. For example, programs in Portugal that teach social-emotional skills in schools have effectively reduced mental health issues, particularly for disadvantaged students.
However, challenges remain. More than half of U.S. schools report being unable to hire enough licensed professionals to meet the growing demand. Additionally, many of these programs rely on grants or Medicaid funding, which are vulnerable to political and budget changes. And lack of communication between health and education systems makes it difficult to track progress and outcomes, which could threaten funding, especially under outcomes-based models.
Programs like England’s Crisis Resolution Teams (CRTs), which provide intensive at-home support during mental health crises, have been shown to lower hospital admissions and reduce costs. These teams meet people where they are, de-escalate crises, and connect them to ongoing care. Community-based approaches have demonstrated similar benefits in the United States through pilot projects, reaching people who might not otherwise seek help. Yet these efforts face funding instability and depend on collaboration between healthcare, education, and community organizations.
Taking therapy to where people already are, like schools, community centers, or even home crisis teams, is both impactful and feasible. These approaches are highly effective at reducing mental health symptoms and preventing crises, particularly for youth and underserved populations. However, achieving long-term success requires stable funding, policy changes, and partnerships between sectors.
For therapists, this is a clear opportunity to engage. Advocate for sustainable funding, explore ways to collaborate with schools and community organizations, and help expand access to care, one step at a time. By stepping into these spaces, you can bring meaningful change to individuals and communities.
4. Big system reforms
While only a small fraction of therapists (3%) called for a complete system overhaul, it’s worth looking at what other countries do. Models in England and New Zealand use integrated systems with global budgets to control costs and improve access.
Countries with single-payer or integrated systems often achieve better cost control and broader access. Still, they are not without issues like long wait times and equity challenges.
New Zealand and England, for example, have decades of experience with universal healthcare systems. Yet, both nations still face political debates and implementation challenges. For instance, New Zealand recently eliminated its Māori Health Authority, aiming to fold its responsibilities into the larger national health system. While proponents argue this could enhance health equity for the Māori population, critics worry this change might fail to address deeper institutional disparities. This highlights that even longstanding universal systems require continual adjustments and political negotiation.
Implementing such a system in the United States would be extraordinarily difficult. The fragmentation of the current system poses major obstacles, including the integration of records, policies, and payment systems. Politically, moving to a single-payer or centralized system would require broad public support and coordinated policy changes, both of which are challenging in the U.S. Furthermore, these reforms demand significant investment of time and resources, with no guarantees of immediate success or stability.
A full healthcare system overhaul is unlikely in the near future for the U.S. However, smaller-scale experiments, like piloting global budgets at the state level, could offer valuable insights. Incremental changes may pave the way for broader reforms while addressing specific issues more effectively.
5. Better access to telehealth
The pandemic made telehealth a household name, but only 2% of therapists listed it as a top solution. Yet, the data shows it’s a powerful tool for access.
Telehealth has become an invaluable tool for expanding access to therapy. It allows therapists to reach clients who may otherwise be unable to attend in-person sessions due to transportation barriers, mobility issues, or living in remote areas.
Research consistently shows that telehealth is just as effective as in-person therapy for most conditions, and clients report high levels of satisfaction even in cases where video calls transition to audio-only due to technical difficulties.
However, its potential is limited by persistent challenges, such as the digital divide. Millions of Americans, especially in rural and low-income areas, lack reliable high-speed internet, which makes telehealth inaccessible for them.
Expanding subsidized broadband access is crucial to ensuring telehealth improves equity rather than reinforcing disparities. Another concern is payment parity: therapists worry that insurers may reduce reimbursement rates for telehealth, which could discourage its use.
Advocating for policies that ensure telehealth sessions are reimbursed at the same rate as in-person care is essential. Additionally, licensing laws restrict cross-state practice, although efforts like PSYPACT provide promising solutions. With the right infrastructure, regulatory protections, and support for technology access, telehealth can continue to thrive as a scalable, high-impact solution for therapists and their clients.
6. Improving cultural and language access
Though only 1% of therapists named it, improving cultural and language access in therapy is critical for equity and better care outcomes. Culturally and linguistically matched care means delivering services in a client’s preferred language and within their cultural context, provided by diverse, bilingual, and culturally competent professionals. Data shows that this approach reduces dropout rates, strengthens trust, and improves care outcomes. When clients cannot see themselves reflected in their providers or are unable to communicate in their preferred language, they are less likely to seek treatment or remain engaged in care.
Research supports the effectiveness of culturally and linguistically appropriate interventions. For instance, the failure of the Affordable Care Act’s Medicaid expansion to increase care for Black adults highlights that financial barriers are not the only issue; trust and cultural understanding also play a major role.
To address these gaps, many successful strategies have emerged. Community health workers who share the same background as their clients help build trust and strengthen connections to care. Similarly, higher Medicaid reimbursement rates for bilingual providers in states like New York incentivize the development of culturally informed care.
Despite these promising examples, there are significant challenges. Language services are often not reimbursed by insurers, leaving the financial burden on providers and agencies. Additionally, the shortage of therapists is exacerbated when focusing on bilingual and minority providers. For example, only 5.5% of U.S. psychologists are bilingual Spanish speakers, far short of the need.
However, scaling these efforts is difficult due to systemic barriers. Workforce pipeline issues remain a major challenge, as too few therapists from underrepresented backgrounds reach licensing and certification stages. Insurance reimbursement gaps further discourage these efforts, as language services and cultural expertise often go unpaid despite their clear impact.
To make meaningful progress, we must invest in developing a diverse workforce of therapists. This includes recruiting and training more clinicians from underrepresented racial, ethnic, and linguistic backgrounds, as well as advocating for better reimbursement policies that value bilingual and culturally trained providers.
Simple, near-term interventions, such as cultural competency training for providers or integrating community health workers who reflect the populations they serve, can also help bridge the gap. The evidence is clear that culturally informed care improves engagement and outcomes, but achieving lasting equity requires sustained advocacy, policy changes, and systemic commitment. Providers can play an active role by championing these changes and continually improving their ability to meet the diverse needs of their communities.
What’s the takeaway for therapists?
No single solution is a silver bullet. The most feasible path is a multi-layered approach where insurance reform, cost reduction, and new care models work together, each addressing a different layer of the access puzzle.
- Advocate for strong reimbursement and enforceable network rules so more therapists can join insurance and serve more clients.
- Support local partnerships. Community and school care can change lives where it happens, especially with reliable, braided funding streams.
- Push tech equity and payment parity for telehealth, since it’s now an indispensable tool.
- Promote diversity, bilingual hiring, and cultural training within your organization or practice.
Improving access means stacking strategies and fighting on several fronts, from the policy arena to your own waiting room. Understanding what works, and why, makes you a more powerful advocate for your clients and your profession.